Although it’s relatively new, endovascular neurosurgery is being used to treat an increasing number of health problems — with remarkable results. Through research and collaboration, experts from a variety of fields are coming together to innovate a type of surgery that is helping some of the highest risk patients.
What is Endovascular Neurosurgery?
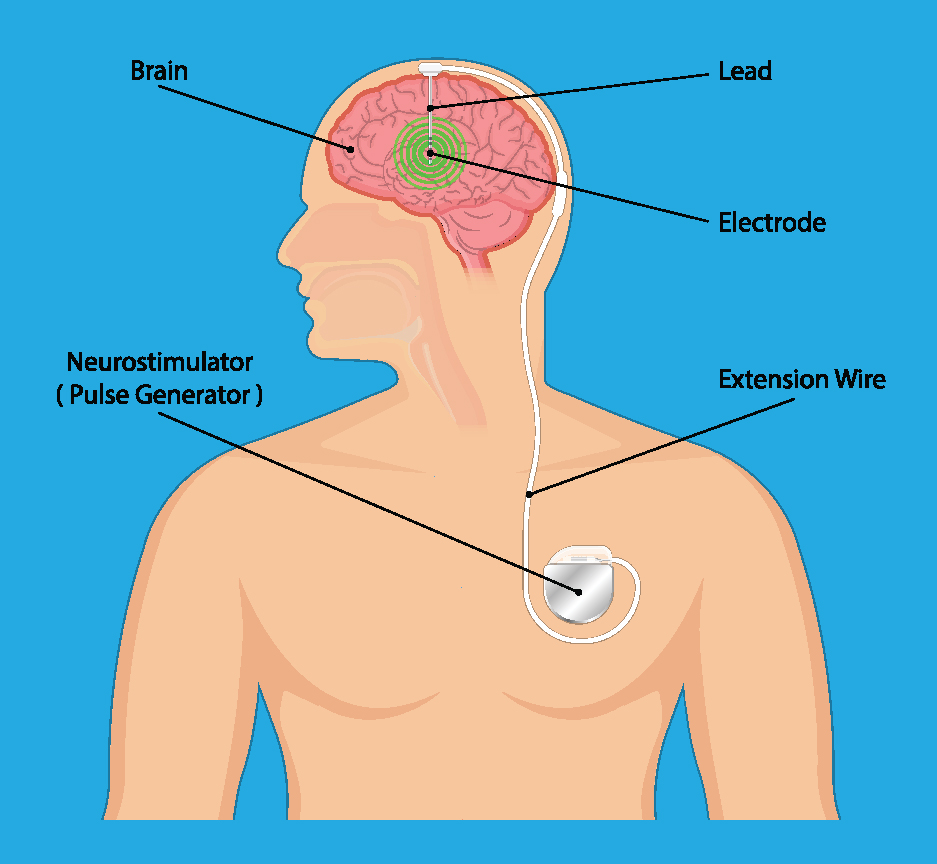
Endovascular neurosurgery is a subspecialty of neurosurgery that combines multiple types of expertise. Incorporating both neurosurgery, which treats conditions of the brain and nervous system, and interventional radiology, which uses imaging and minimally invasive techniques to diagnose and treat injuries and health conditions, endovascular neurosurgery uses small catheters to diagnose and treat health problems affecting the brain and spinal cord.
What Conditions Endovascular Neurosurgery Treat?
Endovascular neurosurgery can be used to diagnose and treat a variety of injuries, diseases and health conditions including:
- Strokes
- Brain aneurysm
- Cerebrovascular malformations including arteriovenous malformations (AVMs) and dural arteriovenous fistula (dAVF)
- Carotid artery disease
- Atherosclerosis (narrowing) of the vessels of the brain
- Idiopathic intracranial hypertension (formerly pseudotumor cerebri)
This is merely a partial list of the many health concerns that can be addressed with endovascular neurosurgery — a list that will continue to grow as neurosurgeons, interventional radiologists, and interventional neurologists work together to advance the science surrounding these techniques.
What Are the Benefits of Endovascular Neurosurgery?
The blood vessels of the brain are deep within the brain itself, meaning they’re not readily accessible without open surgery. Because it involves the use of catheters to pass through blood vessels, endovascular neurosurgery is a minimally invasive technique that provides an alternative to more invasive options.
Rather than opening the skull to get into the brain, endovascular neurosurgeons often only need to make a tiny puncture to insert the catheters they use in surgery.
The minimally invasive nature of endovascular neurosurgery means that some patients who receive elective (non-emergency) types of this procedure can go home the same day.
Even in cases where recovery takes a little longer, patient outcomes are generally very good. Many people can go home within one day of surgery and are back at work within a week.
Another major benefit of endovascular neurosurgery is that it offers hope for people with diseases or conditions that would have been otherwise untreatable. These are patients who didn't have a different treatment option — or at least a good treatment option — and these endovascular techniques are allowing neurosurgeons to provide life-altering or even life-saving care for them.
Advancing Technology, Saving Lives
Endovascular neurosurgery is an exciting field that allows surgeons to greatly improve outcomes for patients who were otherwise at the mercy of their disease.
Treatment options that weren’t available only a few decades ago are now saving people’s lives — and will continue to do so as the field grows and expands through continued collaborative research and innovation.
If you or a loved one is seeking treatment for a condition of the spine, or to schedule an appointment with any of our MHSI experts, visit www.mhsi.com/appointments or call 248-784-3667.