As adults age, it’s very common that the loss of space between the neck’s cervical vertebrae may begin to wear down – causing cervical disc degeneration. These cervical discs begin to collapse and bulge; they may become herniated, or, even compress nerves within the neck affecting one’s shoulders, arms, hands or legs.
Michigan Head & Spine Institute, Author at Michigan Head & Spine Institute Blog - Page 7 of 8
Over two-thirds of individuals experience chronic low back pain (LBP) in their lifetime, according to the New England Journal of Medicine. Some of the most common causes of low back pain include the biochemical degeneration of the intervertebral disc (IVD), spinal stenosis, and disc herniation. For these individuals, posterolateral and interbody fusion techniques are frequently considered for those with one- or two-level degenerative disc disease whose symptoms are unresponsive to conservative treatment. Nevertheless, pre-operative diagnostic techniques that may identify those patients with degenerative disc disease without significant neurological compression who may benefit from surgical intervention remain elusive.
Henry C. Tong, M.D. of MHSI and his colleague at Oakland University William Beaumont School of Medicine, Mengqiao Alan Xi, BSc, recently published their research that re-evaluated the effectiveness of lumbar discography with post-discography CT.
Their study results indicate that discography with post-discography CT can be an effective method to evaluate patients with discogenic back pain refractory to non-operative treatments. Those patients with one- or two-level high concordant pain scores with associated annular tears and negative control disc represent good surgical candidates for lumbar interbody spinal fusion.
To read the full study, click this link.
Every 40 seconds someone has a stroke, and every four minutes someone in the U.S. dies from a stroke. Stroke is the leading cause of disability in the U.S. and the #5 cause of death. One out of six people will suffer a stroke in his or her lifetime. Are these statistics enough to make you ask – “what would I do if my loved one was having a stroke?”
The American Heart and Stroke Associations say to remember the signs of a stroke this way: F=face drooping, A=arm weakness, S=speech difficulty and T=time to call 911. Remembering FAST could make the difference between life and death or the difference between a full recovery and a permanent disability.
What is a Stroke?
There are three types of stroke:
1. Ischemic stroke occurs when a blood clot obstructs a blood vessel supplying blood to the brain and deprives the brain of blood flow. It is accounts for 87% of stroke cases.
2. Intracranial hemorrhage occurs when a weakened blood vessel ruptures, usually due to high blood pressure. The mass of blood from the ruptured artery pushes on the normal brain, reducing its blood flow and can directly damage the brain.
3. Subarachnoid Hemorrhage is a type of hemorrhagic stroke in which a weakness in the wall of a blood vessel dilates and bursts. These weakened blood vessels are called aneurysms and arteriovenous malformations or AVMs. Intracranial and subarachnoid hemorrhage account for about 13% of stroke cases.
4. A Transient Ischemic Attack (TIA) is often referred to as a “mini-stroke” and is caused by a temporary clot that prevents blood flow to the brain. They can be a predictor of a more serious stroke to occur in the future.
How is a Stroke Treated?
The good news is that most strokes can be treated if bystanders recognize the symptoms and react quickly to get the stroke victim to the emergency room.
Doctors in areas where stroke specialists are not on-site use the tools of the Stroke Network to connect with stroke experts as they treat patients in their emergency rooms. This provides the patient with the best possible outcome.
For an Ischemic stroke that treatment might include tissue plasminogen activator (tPA).
tPA is a clot busting drug which must be given within 3 to 4.5 hours from the first signs of a stroke. If the drug does not reduce the clots, minimally invasive surgery is required to remove the clots. This is generally performed by a neurosurgeon, who is a neuroendovascular specialist. These endovascular procedures are minimally invasive and often the patient is home anywhere from the same day to two days later.
Rehabilitation After A Stroke
Patients who do suffer a stroke can require physical rehabilitation. At Michigan Head & Spine Institute, physiatrists – physical medicine and rehabilitation doctors have the expertise to work with stroke patients to return each person to being able to function to the fullest extent possible.
For those who require rehabilitation, a consult with an MHSI physiatrist for stroke rehabilitation can be scheduled by calling 248-784-3667.
 In her early thirties, Amy experienced very bad and massive migraine headaches. At that time, she went to see a neurosurgeon and was diagnosed with Chiari I malformation. Amy was told she could have brain surgery, but it was an elective surgery. She was told if it’s not bothering you – you shouldn’t fix it. Fast forward to now at age 43.
In her early thirties, Amy experienced very bad and massive migraine headaches. At that time, she went to see a neurosurgeon and was diagnosed with Chiari I malformation. Amy was told she could have brain surgery, but it was an elective surgery. She was told if it’s not bothering you – you shouldn’t fix it. Fast forward to now at age 43.
Amy is a kindergarten teacher of 27 students in her classroom. She would be exhausted and fight to stay awake. Everyday would be a challenge because of fatigue, headaches, and continuous scratching herself to stay awake. Five minutes driving in the car would be very stressful for her and falling asleep at the wheel was becoming a serious issue for Amy.
Chiari malformations are structural defects that occur in the cerebellum, the part of the brain that controls coordination and muscle movement. Previous estimates were that malformations occur in about one in every 1,000 births, but increased use of diagnostic imaging indicates that the disorder may be more common than once thought.
What is Chiari Malformation?
Holly Gilmer, M.D., neurosurgeon and a leading expert in Chiari malformation explains that older children experience headaches, dizziness, ringing in the ears, and problems with vision. One of the most frequent presentations is scoliosis with none of these symptoms except infrequent headaches. Some children may not have noticeable symptoms until adolescence or adulthood. In teen and adult years, problems can include persistent headaches, neck pain, and weakness and/or numbness and tingling in the arms and legs.
Adult symptoms include neck pain, balance problems, muscle weakness, numbness or other abnormal feelings in the arms or legs, dizziness, vision problems, difficulty swallowing, ringing or buzzing in the ears, hearing loss, vomiting, insomnia, or headache made worse by coughing, laughing, or straining. Hand-eye coordination and fine motor skills may be affected. Symptoms can change over time depending on the build-up of cerebrospinal fluid and pressure on the brain, spinal cord, and nerves.
Dr. Gilmer says that “surgical treatment to correct the compression involves removing a portion of the skull and usually part of the C1 vertebra. The cerebellar tonsils are usually partially removed. We always open the covering of the brain (dura) and use an expansion graft to make the dura larger and give the brain more room to expand.”
“It only takes one person to change your life and I’m very grateful to Dr. Gilmer and Michigan Head & Spine Institute,” says Amy.
To refer a patient for diagnosis of Chiari malformation or evaluation for decompression surgery, call 248-784-3667.
by Daniel B. Michael, M.D., Ph.D., Emeritus and Retired Neurosurgeon
Everyone forgets, from the day we are born until we die. Memory is one of the most important functions our brains provide. When we forget or cannot recall an event, person or thing it can be frustrating. When such memories can never be recalled it can be life threatening. Alzheimer Disease (AD) is the progressive loss of certain types of memory due to specific degenerative changes in the brain. Twelve years following the diagnosis, over 95% of AD patients are dead. Alzheimer Disease is fatal and currently there is no effective treatment. In 2012 there were 5.4 million estimated cases of AD with approximately 36 million cases worldwide. The incidence is expected to quadruple by 2050. In 2012 US the cost to care for AD patients was estimated to be $200 Billion; in 2050 the cost will increase to an estimated, $1.2 Trillion, 70% paid for by Medicare. Unless effective treatments for AD can be found we face an unprecedented healthcare crisis. Dr. James Fontanesi, a noted radiation oncologist then on staff at William Beaumont Hospital (WBH), Royal Oak, MI, observed that relatively low doses of external radiation had been used to treat abnormal deposits of amyloid in parts of the body other than the brain. Amyloid deposition in the brain has been thought to play an important role in the development of AD. He hypothesized that radiation could be used to reduce amyloid in the brains of AD patients and lead to improved memory function. Over the past five years Dr. Fontanesi gathered a team of radiation oncologists, radiobiologists, and behavioral psychologists to design and carry out animal laboratory studies to see if radiation would reduce amyloid in the brain, improve memory, and if so by what mechanisms this treatment worked. Daniel Michael, M.D., MHSI neurosurgeon and neuroscientist, was part of this team, providing help in experimental design and analysis. The MHSI board of directors voted to provide grant money to support this research.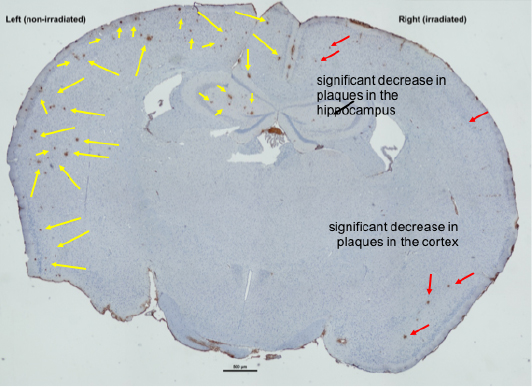 The research used a transgenic mouse model of AD. Early experiments subjecting one half of the mouse’s brain to radiation demonstrated in dramatic fashion that amyloid could be reduce using this treatment (see figure). Subsequent studies suggested the best dose of radiation to use and possible mechanisms by which the radiation reduced amyloid. Whole brain radiation mouse studies then provided evidence that radiation improved memory in the AD mice. The results of these studies have been reported at radiation oncology, AD and neuroscience meetings worldwide. In November 2015, the results of these experiments were reported in the peer reviewed journal, Radiotherapy and Oncology (Marples B, McGee M, Callan S, Bowen SE, Thibodeau BJ, Michael DB, Wilson GD, Maddens ME, Fontanesi J, Martinez AA: Cranial irradiation significantly reduces beta amyloid plaques in the brain and improves cognition in a murine model of Alzheimer's Disease (AD). Radiother Oncol. 2015 Nov 23. pii: S0167-8140(15)00568-X. doi: 10.1016/j.radonc.2015.10.019. [Epub ahead of print] PMID: 26615717). These animal studies have provided the basis for a Phase 1 human safety trial of radiation in AD patients. This trial has been developed in cooperation with the FDA. It is currently undergoing institutional review board scrutiny and is expected to enroll the first AD subjects in 2016. In addition to members of the team from Beaumont Hospitals and 21st Century Oncology, Mary Martin, RN, Dr. David Lustig, M.D., neurologist, and Dr. Michael all from MHSI will be participating in this exciting study. MHSI is proud to continue its support of research which we hope will lead to an effective treatment for AD.
The research used a transgenic mouse model of AD. Early experiments subjecting one half of the mouse’s brain to radiation demonstrated in dramatic fashion that amyloid could be reduce using this treatment (see figure). Subsequent studies suggested the best dose of radiation to use and possible mechanisms by which the radiation reduced amyloid. Whole brain radiation mouse studies then provided evidence that radiation improved memory in the AD mice. The results of these studies have been reported at radiation oncology, AD and neuroscience meetings worldwide. In November 2015, the results of these experiments were reported in the peer reviewed journal, Radiotherapy and Oncology (Marples B, McGee M, Callan S, Bowen SE, Thibodeau BJ, Michael DB, Wilson GD, Maddens ME, Fontanesi J, Martinez AA: Cranial irradiation significantly reduces beta amyloid plaques in the brain and improves cognition in a murine model of Alzheimer's Disease (AD). Radiother Oncol. 2015 Nov 23. pii: S0167-8140(15)00568-X. doi: 10.1016/j.radonc.2015.10.019. [Epub ahead of print] PMID: 26615717). These animal studies have provided the basis for a Phase 1 human safety trial of radiation in AD patients. This trial has been developed in cooperation with the FDA. It is currently undergoing institutional review board scrutiny and is expected to enroll the first AD subjects in 2016. In addition to members of the team from Beaumont Hospitals and 21st Century Oncology, Mary Martin, RN, Dr. David Lustig, M.D., neurologist, and Dr. Michael all from MHSI will be participating in this exciting study. MHSI is proud to continue its support of research which we hope will lead to an effective treatment for AD.
 Parents are very intuitive to the developmental growth of their children and how they progress as a baby, toddler, pre-schooler, to elementary age. Since an infant, Zeke’s mom, Deb, knew something was wrong for a longtime.
Parents are very intuitive to the developmental growth of their children and how they progress as a baby, toddler, pre-schooler, to elementary age. Since an infant, Zeke’s mom, Deb, knew something was wrong for a longtime.
He walked on his toes constantly – he never walked on his flat feet. He felt no hot or cold. Zeke had periods of rage and irritability. And as may Chiari patients, his speech was impeded by a thick tongue. Then one day during lunchtime, he had a one pupil that was dilated very large. A visit to the eye doctor indicated that there was extreme pressure on Zeke’s retina – pressure that was coming from the brain. An emergency trip was made to the ER and it was then doctors diagnosed Zeke as having Chiari malformation.
Zeke’s mom did extensive research about Chiari malformation. She communicated with many patients who had great surgical outcomes and one name kept coming up, Dr. Gilmer, located in Royal Oak, Mich.
“She found me on the internet,” says Holly Gilmer, M.D., neurosurgeon. “She did her research, searching all opportunities, and was very particular about what she wanted for Zeke She found that I specialize in Chiari malformation surgery.”
Deb says, “Zeke and his family traveled from Maine and we’re so glad we found Dr. Gilmer.”
What is Chiari Malformation
Chiari malformations are structural defects that occur in the cerebellum, the part of the brain that controls coordination and muscle movement. Previous estimates were that malformations occur in about one in every 1,000 births, but increased use of diagnostic imaging indicates that the disorder may be more common.
Normally the cerebellum and parts of the brain stem sit in the posterior fossa of the skull, above the foramen magnum, or the opening to the spinal canal. In individuals with Chiari malformations, the posterior fossa is abnormally small and misshapen. It presses on the brain, forcing it downward and causing the cerebellar tonsils to protrude into the spinal canal. This blocks the flow of cerebrospinal fluid to the brain, which can lead to hydrocephalus and/or increased intracranial pressure. It also causes direct pressure on the brain stem and upper spinal cord.
Chiari malformation is diagnosed by MRI. When deciding if surgery is an option, the extent of the herniation of the brain into the spine is not as important as the symptoms the patient experiences. For some adults, symptoms are not severe and they do not require surgery. Chiari malformation is also sometimes an incidental finding on MRI, and the person is asymptomatic.
What you see in the movies just may bring a spotlight on the issue of concussion prevention and diagnosis that Daniel Michael, M.D., PhD., has been treating, studying and teaching on for several years. As a co-author of an article published on October 2014 titled Concussion 101, in the Neurosurgery journal, Dr. Michael and his colleagues indicated that prevention, accurate diagnosis, and prompt management of concussions require that players, parents, coaches, and medical personnel to be accurately educated on current concussion data and guidelines.
By combining various program methods and offering a concussion education program in health classes for all students, as opposed to only athletes, leads to a more educated public and will result in responsible actions being taken when concussion is suspected.
The ThinkFirst program aims to help achieve this goal by providing classroom presentations. The ThinkFirst Foundation holds monthly online training for injury prevention coordinators interested in operating a ThinkFirst chapter within a hospital or other medical setting for providing ThinkFirst educational programs to schools and other community groups.
LEARNING ABOUT CONCUSSIONS FROM OTHER’S EXPERIENCES
Voices for Injury Prevention speakers are individuals who have experienced a traumatic brain or spinal cord injury themselves and share their personal story with students to help them realize the ramifications of such injuries and the importance of prevention. Student evaluations have shown that students are significantly more influenced to choose safe behaviors when they have heard from someone who has experienced a brain or spinal cord injury, as opposed to hearing the facts on injury or potential for being ticketed through law enforcement.
Data demonstrated that the program was efficacious in changing student attitudes about safety and that these attitudes persisted out to 3 months after the presentation.
Founded by neurosurgeons in 1986 with the support of the American Association of Neurological Surgeons and the Congress of Neurological Surgeons, the ThinkFirst National Injury Prevention Foundation website has studies on its programs and contact information for the 150 national chapters and 39 international chapters.
Source:
Neurosurgery:
October 2014 – Volume 75 – Issue – p S131–S135
doi: 10.1227/NEU.0000000000000482

This year’s holiday party honored a beloved colleague, husband and father – Dr. Daniel Pieper who passed away in May of 2015. He left behind his beloved colleagues and his wife Donna, his children Stephanie, Lindsey, Brett, John Paul, and Michelle. His family is the ultimate legacy, the loving husband and father.
His fellow physicians at Michigan Head and Spine Institute, the staff he worked closely with for several decades and colleagues throughout Beaumont Hospital and St. John Providence Health System continue to grieve at the loss of a friend. Dr. Perez-Cruet, on behalf of these colleagues shares, “Dan will forever be in our hearts and on our minds – he’s made an indelible mark on each of us personally and professionally. He was an extraordinary neurosurgeon, husband, father and friend.”
As many of his colleagues share, he was an outstanding neurosurgeon who positively changed the lives of his patients. He was one of a very few of neurosurgeons in the United States who through his expertise for treating peculiar and complicated brain tumors, created techniques and developed instruments he used to treat these difficult tumors. He’s left a legacy of medical expertise to his students and fellow neurosurgeons.
Dr. Pieper also changed the lives of many individuals in foreign countries, particularly the mission trips to the Davao City, Mindanoa, in the southern Philippines. Judith Hack, his long-time nurse and co-pilot on these trips shares there was a great need for neurosurgical/craniofacial assistance for the repair of Meningioencephaloceles, which is a congenital facial anomaly. Dr. Pieper donated his time and skills so that these patients would not be forced to live with severe facial disfigurement.
In 2013 at age one, a courageous and free-spirited little girl from Arizona named Zion was diagnosed with Chiari Malformation (CM), Type 1 (a brain abnormality that causes the cerebellum, the part of the brain that controls coordination and muscle movement, to cut into the space normally used by the spinal cord, causing pressure on the brain stem and blocking flow of cerebrospinal fluid to the brain).
Nikkita Smith-Dennis, mother of little Zion, did what every mother would do when faced with such a challenge and launched an exhaustive research effort to find the best physician and medical treatment to help her daughter. After extensive online research and several physician visits, Smith-Dennis focused her attention on Detroit and Holly S. Gilmer, M.D., a nationally-renowned pediatric neurosurgeon at Michigan Head & Spine Institute in Southfield, MI.
“Since her birth in August 2012, Zion’s medical journey began,” stated Nikkita Dennis. “She was not meeting her developmental milestones and in February of 2013 she was diagnosed with Chiari Malformation. I did everything in my power to learn about CM and the effects and challenges it would have on her life and that research led me directly to Dr. Gilmer,” she added.
Dr. Holly Gilmer is the leading expert on CM and only neurosurgeon in Michigan to perform Chiari decompression surgery—a rare procedure involving the removal of part of the skull.
In January 2015, little Zion and her family made their journey from warm Phoenix to wintery Southfield, where she underwent her second and finally a successful decompression surgery for Chiari Malformation performed by Gilmer.
“Of more than 200 patients on whom I have performed decompression surgery for Chiari, 100% have noted they experience less, or none, of their previous symptoms, and we expected the same for Zion,” said Dr. Gilmer, who is one of only five female neurosurgeons in the state of Michigan, and, only one of a very few neurosurgeon in Michigan performing decompression for CM.
Zion has had to endure two major brain surgeries – and she is not yet three years old. From the time of her birth to now, Zion has had an incredible amount of medical challenges – already enough for anyone to sustain in a lifetime.
On May 7th, Zion and her family will be back at Michigan Head and Spine Institute for a follow-up visit with Dr. Gilmer. Through her daughter’s journey Nikkita Dennis has become a passionate advocate for CM, raising awareness in their hometown and online with an artistic mural project named “One Face of Many.” Little Zion is the subject of the inaugural mural campaign and the Dennis family is bringing the project to Detroit – building awareness for much needed funds to help other families travel to Michigan so their loved ones can have Chiari Decompression Surgery.
This incredible journey has inspired me to start a nonprofit organization called Zion’s Chiari Children’s Foundation in an effort to build awareness of this medical condition and help provide medical and travel grants for families who want their children to obtain the best medical care, says Dennis.
[CLICK HERE to view Channel 4’s News Story]
[CLICK HERE to learn more about Chiari Malformation]
###
Editor’s Note: Infants may have symptoms from any type of CM and may have difficulty swallowing, irritability when being fed, excessive drooling, a weak cry, gagging or vomiting, arm weakness, a stiff neck, breathing problems, developmental delays, and an inability to gain weight. Adult Symptoms may include: neck pain, balance problems, muscle weakness, numbness or other abnormal feelings in the arms or legs, dizziness, vision problems, difficulty swallowing, ringing or buzzing in the ears, hearing loss, vomiting, insomnia, depression, or headache made worse by coughing or straining. A MRI is the gold standard for diagnosing Chiari Malformation.
Patients frequently have many questions regarding insurance coverage and billing. Because each person’s insurance coverage is different, we’ve asked Melissa Riemer, billing department manager, for a few general tips to help patient’s better understand their bills:
- When reviewing the Explanation of Benefits (EOB) from your insurance carrier, match it up to the bill or receipt for same date of service. Doing so will ensure the EOB is addressing the service provided, thus reducing confusion about the service.
- If you know your copays and deductibles, the bill will make more sense and you’ll know what to expect will be your portion of payment in advance and then when receiving the bill.
- Understanding when your specific insurance requires an authorization or a physician referral prevents appointments needing to be rescheduled. By the time you receive the bill, the insurance company has already approved the visit or procedure reducing phone calls back to the insurance company.
- To prevent bills from aging and causing debt issues for our patients, when you pay a bill that sum is applied to the oldest service date first. This keeps your account in a more current status.
- If you should you have difficulty paying your balance, don’t ignore the invoice. Contact the Billing Department at 248-869-3981 sooner than later. By doing so it is easier to set up a payment plans that work for everyone.
Just like you, the Billing staff does its best to keep up with changes to your current insurance policies, coverages and payment plans. As a patient, it is important you know what your policy covers, including copays and deductibles, this helps prevents the anxiety of unexpected financial obligations.