Every year, around 2.9 million cases of traumatic brain injury (TBI) occur in the United States, and about 5.3 million Americans are currently living with a disability related to a traumatic brain injury.
Understanding traumatic brain injuries —symptoms, treatment options and how to prevent them — can help prepare you in the event you or a loved one sustain this type of injury.
What is a Traumatic Brain Injury (TBI)?
Any injury with an external cause that affects how the brain works is a traumatic brain injury, often abbreviated to TBI. These injuries are typically caused by a blow to the head — like a fall, or a car accident where the head hits the steering wheel at high speed — or a penetrating injury such as a gunshot wound.
A traumatic brain injury can be mild, moderate or severe. Fortunately, about 75 percent of traumatic brain injuries are mild. The most common type of mild traumatic brain injury is a concussion.
Symptoms of a traumatic brain injury may include:
- Amnesia
- Confusion
- Trouble concentrating
- Difficulty speaking or understanding language
- Inappropriate expression of emotion, either laughing or crying
- Aggression and irritability
- Blurred vision
- Slurred speech
- Dilated or unequal pupils
- Headaches
- Ringing in the ears
- Nausea or vomiting
- Anxiety
- Problems with balance
People who have suffered a traumatic brain injury may also experience symptoms of post-traumatic stress disorder (PTSD) alongside those of their injury.
It’s important for athletes, fall-prone individuals (like persons with disabilities or who are elderly) or anyone else who may be vulnerable to a traumatic brain injury to know the signs and symptoms, so they can seek care immediately upon noticing them.
Treating Traumatic Brain Injuries
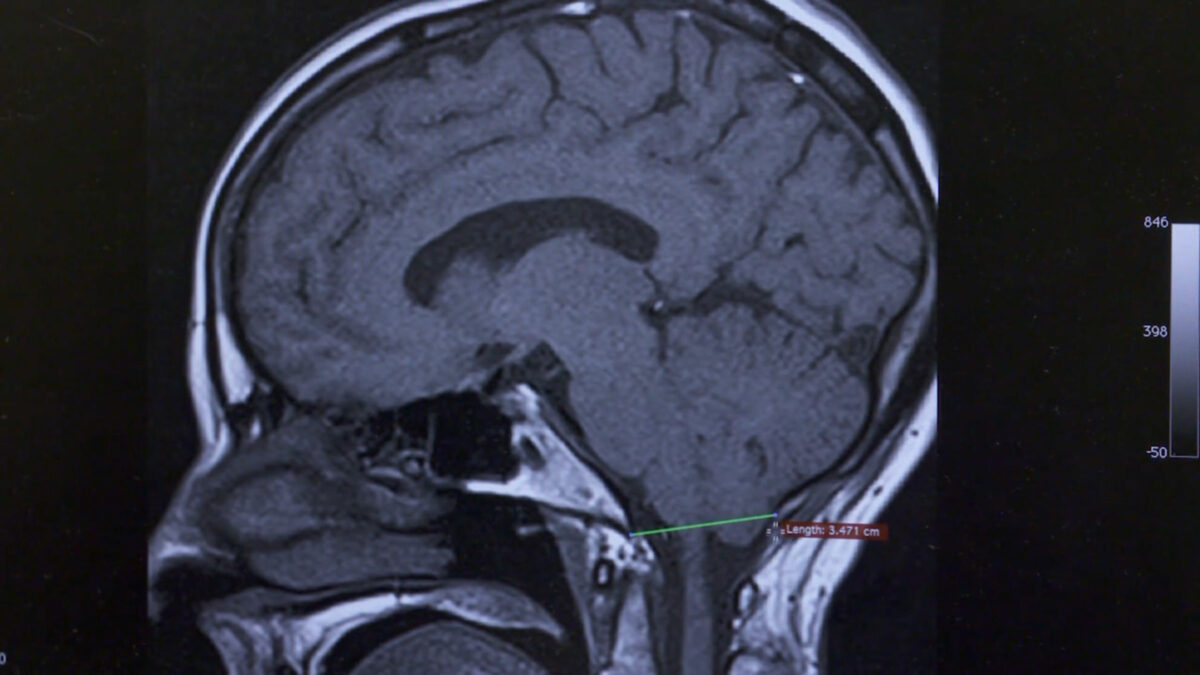
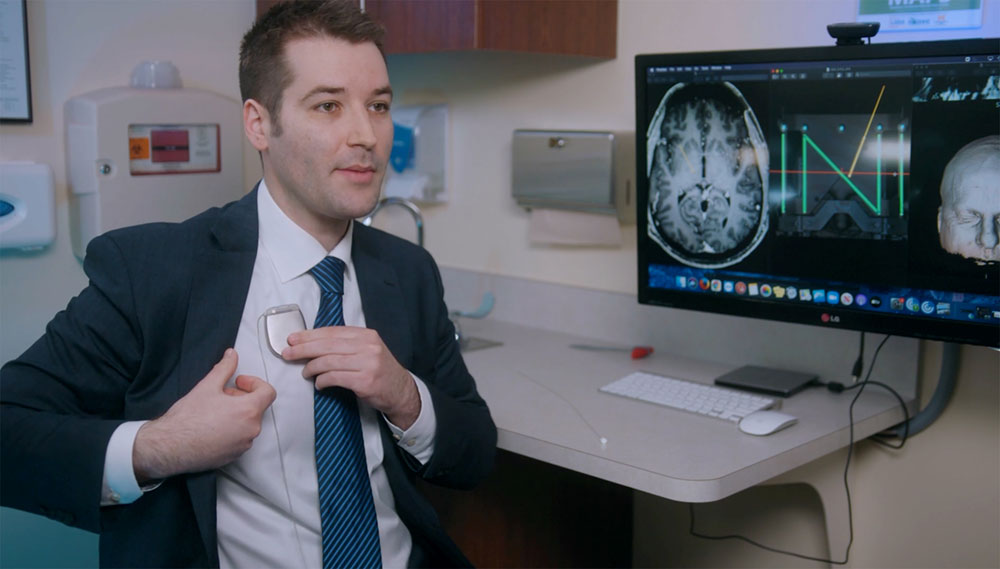
Many people with TBIs — particularly mild ones such as concussion — will be first seen and treated by their primary doctor or an urgent care provider. Then, depending on the severity of the injury, they may be referred to a specialist — like a neurologist or neurosurgeon — for further evaluation and treatment.
In the case of mild traumatic brain injuries, recovery often involves rest and over-the-counter pain relievers, and can be done at home. Moderate traumatic brain injury typically requires more intensive treatment such as surgery.
What to Expect After a Traumatic Brain Injury
Most people who sustain a mild traumatic brain injury will stop having symptoms within days or weeks. However, up to 25 percent of these people may experience lingering effects such as inability to concentrate, head and neck pain, and memory issues for much longer — possibly months after the event that caused the TBI.
For the small percentage of people who do experience long-term effects after a traumatic brain injury, ongoing treatment is key. Ideally this treatment is overseen by a multidisciplinary team that includes a neurosurgeon, neurologist, and rehab doctor or physical therapist, among other specialists.
Preventing Traumatic Brain Injury
While some TBIs might be more mild or less symptomatic than others, there’s no ideal situation with traumatic brain injury. Every situation is unique and presents its own set of challenges to recovery and treatment.
So how do we prevent TBIs entirely? While you can’t prevent the type of TBIs that come from accidents like tackles on the football field or a car accident, the most powerful tool we have is knowledge. The organization ThinkFirst is an excellent source of trustworthy and comprehensive information on preventing traumatic injuries, offering tips for people of all ages on how to protect the brain.